Selecting the right intraocular lens (IOL) for glaucoma patients requires careful balancing of current visual needs, long-term disease progression, and contrast sensitivity, according to information presented Thursday during glaucoma subspecialty day at the American Academy of Ophthalmology (AAO) meeting in Orlando, Florida.
During her presentation, “Picking Winners: Choosing IOLs in Glaucoma Patients,” Emily Schehlein, MD, a glaucoma and cataract surgeon from Brighton, Michigan, emphasized the importance of evaluating a patient’s ocular history and potential for future progression before selecting a lens. Factors such as patient age, disease stage, fixation involvement, prior surgeries, and comorbidities all influence the suitability of different IOL types, she said.
Dr. Schehlein highlighted three key priorities when planning surgery: setting realistic expectations, achieving precise refractive outcomes, and minimizing ocular surface disease by reducing reliance on drops. “Unhappy patients are almost always the result of mismatched expectations or lack of communication,” she said. “Even a perfect result can feel like a failure if a patient perceives a difference from their expected outcome.”
Reviewing the various IOL categories, Dr. Schehlein noted that monofocal lenses remain suitable for nearly all glaucoma patients, including those with advanced disease or rapid progression. Monovision can be considered with standard IOLs, though it can reduce contrast and binocular summation—both of which can be compromised in glaucoma.
Toric IOLs are useful for correcting astigmatism and improving functional vision. “Even less than one diopter of astigmatism can decrease visual acuity and have an impact on quality of vision,” she said. However, she cautioned not all patients are candidates—concurrent incisional glaucoma surgery, zonular instability, or irregular corneas may limit the benefit of toric IOLs.
Enhanced monofocal lenses can improve intermediate vision with minimal visual disturbances. Dr. Schehlein recommended these options for patients with mild to moderate glaucoma who have stable disease and a healthy ocular surface without other significant ocular comorbidities. Often mini-monovision is used with these lenses which can reduce contrast, but these effects are typically reversible with spectacles.
Figure 2. Key considerations for IOL selection in glaucoma patients include disease stage and progression risk, patient history and comorbidities, surgical planning priorities, and shared decision-making to maximize benefit while minimizing harm.
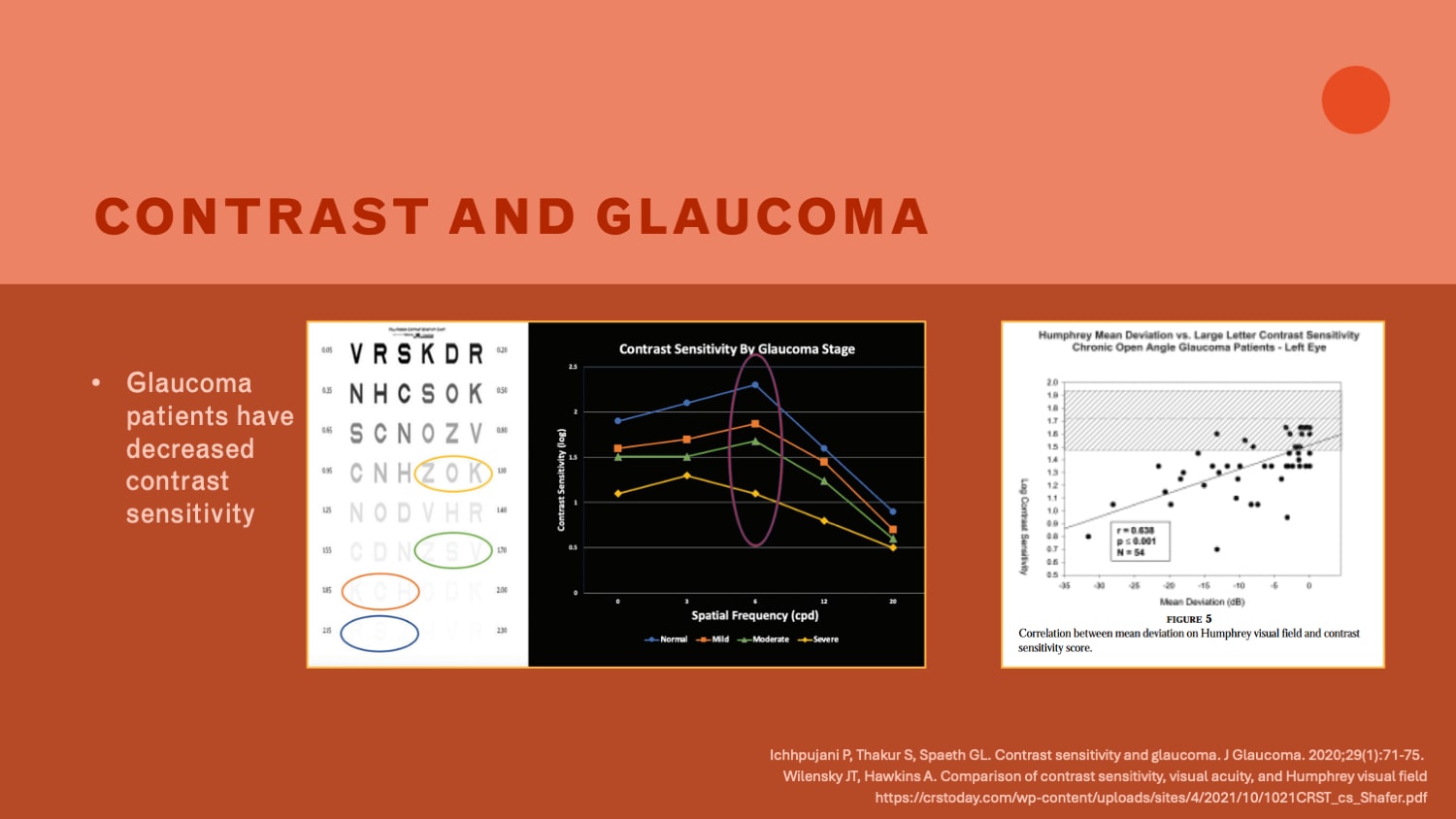
Dr. Schehlein also discussed contrast sensitivity—a key measure of how well patients can distinguish between light and dark areas – and its relation to EDOFs and multifocal IOLs. This is an important consideration when choosing IOLs for patients with glaucoma, as they already tend to have lower contrast sensitivity, which worsens as visual field loss progresses. She cited data showing slight reductions in contrast sensitivity (but not clinically significant) and minor visual field changes with some multifocal and EDOF lenses. Diffractive multifocal lenses present greater risk for contrast reduction and photic phenomena. “When considering multifocal lenses, contrast becomes especially important,” Dr. Schehlein said. “Even small reductions can noticeably affect how well patients function in dim light.” She emphasized that selecting lenses that preserve contrast while meeting visual goals is essential for patient satisfaction.
Dr. Schehlein underscored the importance of assessing disease progression: “Patients with severe fixation-involving glaucoma would likely not benefit from EDOF or multifocal lenses – it is difficult to predict progression in some cases, but we need to be vigilant with patient selection for these types of lenses.”
Setting expectations is critical, Dr. Schehlein reiterated. She advised telling patients, “We’re working with man-made lenses, not the natural lenses that gave them excellent vision 40 years ago. We can’t recreate the vision you had when you were 20, but we can improve what you have today.” Honest discussions about anticipated spectacle dependence, postoperative healing, and potential complications help align patient goals with achievable outcomes.
Looking ahead, Dr. Schehlein expects the use of toric lenses and enhanced monofocals to grow quickly and selective EDOF and multifocal lens use to grow as diagnostic tools continue to improve and physicians are better able to predict the risk of glaucomatous progression. GP








