Laser treatment has been an important and growing part of the glaucoma treatment armamentarium for decades, beginning with argon laser trabeculoplasty (ALT) and then selective laser trabeculoplasty (SLT), which is a mainstay of the contemporary glaucoma practice. However, there remains an unmet need for noninvasive laser treatments that are consistent in both their initial results and duration of effectiveness.
Selective Laser Trabeculoplasty
Laser treatments are not dependent on patient adherence to a daily drop regimen to achieve intraocular pressure (IOP) control. That makes laser a great choice for noncompliant patients, as well as those with ocular surface issues and other reasons for drop intolerance. For these reasons, many glaucoma specialists offer SLT as first-line therapy. Recently, the Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial provided solid evidence that patients could be equally well controlled with either medical or laser therapy.1 Lasers for SLT currently approved in the United States include Solo, Tango, Tango Reflex, Optimis Fusion, and Solutis SLT (Lumibird Medical); Selecta Duet and Selecta Trio (Lumenis); YC-200 S Plus (Nidek); Lightlas SLT Solo (Lightmed); and the Eagle device (Belkin Vision), which was approved in December 2023.
The other advantage of SLT, of course, is the low risk of adverse events. In return for that safety, however, we have accepted limited efficacy. Selective laser trabeculoplasty is successful in reducing IOP by 20% or more in about 70% of patients at 6 months, but the success rate declines to 45% at 1 year and only 27% at 2 years.2 The mechanism by which SLT lowers IOP is thought to be a photochemical reaction, but is not fully understood, so why it stops working is unclear. The short duration of efficacy and variable response are two frustrating aspects of treating this chronic condition.
When SLT fails, glaucoma specialists turn to the option of adding medical therapy, performing a repeat laser procedure, or moving to a minimally invasive glaucoma surgery (MIGS) procedure. When the patient has cataracts, combined phacoemulsification/MIGS procedures can be effective. And, although this decision is always customized to the individual patient, another option is standalone MIGS procedures such as canaloplasty plus goniotomy to achieve the benefits of early intervention in slowing disease progression and preserving vision. However, while these procedures are safer and less invasive than traditional filtration surgery, they are still much more invasive than laser when one is not already entering the eye to perform cataract surgery. Making the jump from laser to a standalone incisional procedure always represents an increase in risk for the patient that must be acknowledged, even if it is justified by the need to reduce IOP.
Femtosecond Laser
Recent innovation in the glaucoma treatment pipeline has the potential to significantly change the risk-benefit calculations for laser vs surgery. Femtosecond lasers are well known for revolutionizing LASIK by allowing surgeons to move from bladed to laser flaps and for innovations in cataract surgery that have led to more precise and repeatable astigmatic incisions and capsulotomies, as well as lens softening before phacoemulsification. However, femtosecond laser also has applications in glaucoma treatment. A new procedure called femtosecond laser image-guided high-precision trabeculotomy (FLigHT) uses a femtosecond laser (ViaLuxe laser system; ViaLase) to create trabecular meshwork (TM) drainage channels without an incision. The noninvasive nature of the procedure has the potential to make the safety profile comparable to SLT. Indeed, in the first-in-human trial of this technology, a 2-year, prospective single-center study, there were no reports of hyphema, IOP spikes, corneal edema, hypotony, peripheral anterior synechiae, or any other device-related serious adverse events.3
The first patients treated with FLigHT were older (mean age of 72.2 years), and two-thirds of the 17 treated eyes had moderate to severe glaucoma. Several aspects of the 2-year study results are of note. First, the eyes were treated with a single 500-µm laser-created channel, compared to the 180° of the TM typically treated in SLT. Even with this limited treatment area, more than 80% of the eyes achieved a ≥20% pressure-lowering effect and maintained it for at least 24 months.3 It is very encouraging to know that a single channel provided the desired effects and that we might be able to get an even larger effect by creating more channels. Larger clinical trials aimed at FDA clearance are under way.
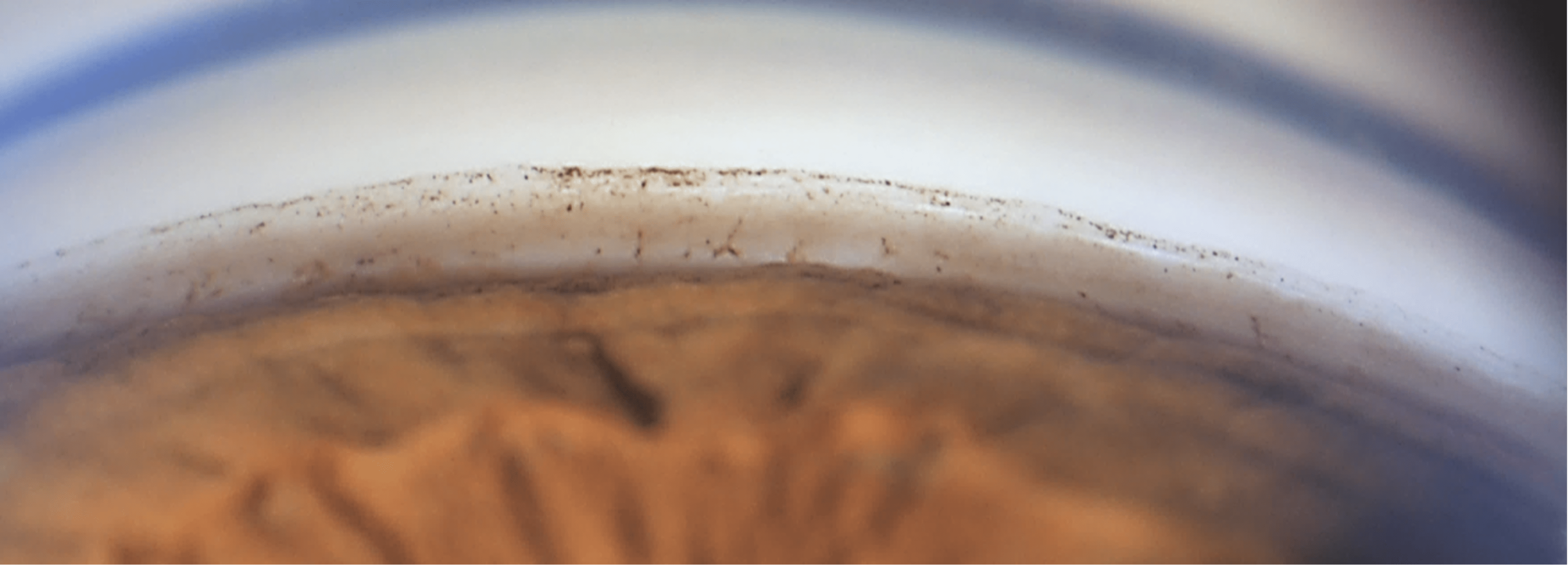
Visualization during the procedure is another important feature and may be partly responsible for these positive outcomes. In a FLigHT procedure, the surgeon creates an opening in the TM, restoring communication to Schlemm’s canal. As that channel is being created by the laser, the surgeon can directly visualize it in real time with ViaLase’s proprietary high-definition gonioscopic and OCT imaging, thus validating the creation of the channel (Figure 1).
Femtosecond laser technology has been successful in cataract practice because it enables surgeons to correct astigmatism in the same predictable fashion, without regard for subspecialty training or years of experience. Similarly, with femtosecond lasers in glaucoma surgery, when the surgeon can see the structures where they are delivering the therapy and precisely control treatment delivery, size, and location, the accuracy and predictability should increase. There are potential advantages for multioffice, multiclinician practices in removing some of the guesswork in glaucoma treatment and standardizing outcomes across clinicians.
Excimer Laser
Used to perform excimer laser trabeculostomy (ELT) (Figure 2), the Elios Vision excimer laser also creates tiny channels in the TM. It is CE marked in Europe and under clinical investigation in the United States. Like femtosecond lasers, excimer lasers are “cold” lasers that minimize heat transfer and collateral damage to surrounding tissues. Excimer laser trabeculostomy requires a corneal incision and insertion of a probe that has to physically touch the TM. It is anticipated to be indicated for use at the time of cataract surgery in the United States. Long-term efficacy results in Europe out to 8 years have been very positive.4

Micropulse Advancements
Micropulse transscleral laser therapy (TLT) has been around for some time, but recent innovations make this noninvasive treatment worth reconsidering for patients across the spectrum of glaucoma severity. The new P3 MicroPulse probe is designed to be used with the Cyclo G6 infrared diode laser (both from Iridex). It has been established that micropulse technology could significantly reduce the amount of energy applied and provide thermal control, but the new probe also modifies the laser treatment so that it is applied more posteriorly, making it even safer. Evidence-based guidelines for patient selection, treatment technique, and expected outcomes have recently been published.5,6
Conclusion
In cataract and refractive surgery, advanced laser technology is appealing to patients. They value innovation and come to our practices seeking the latest and most innovative care that will make procedures safer, more comfortable, or more effective. I, personally, am optimistic that glaucoma patients will similarly embrace new laser technologies once we as clinicians see the data and gain confidence in the results.
It is exciting to see glaucoma continue to evolve from a medication-based subspecialty to an innovation-based subspecialty. Earlier intervention that is effective, noninvasive, and minimizes risk has the potential to help our patients avoid more invasive surgery and, ultimately, maintain good vision for longer. Glaucoma patients deserve a commitment from glaucoma specialists to strive for these outcomes. GP
References
1. Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Laser in Glaucoma and Ocular Hypertension (LiGHT) trial: six-year results of primary selective laser trabeculoplasty versus eye drops for the treatment of glaucoma and ocular hypertension. Ophthalmology. 2023;130(2):139-151. doi:10.1016/j.ophtha.2022.09.009
2. Khawaja AP, Campbell JH, Kirby N, et al. Real-world outcomes of selective laser trabeculoplasty in the United Kingdom. Ophthalmology. 2020;127(6):748-757. doi:10.1016/j.ophtha.2019.11.017
3. Nagy ZZ, Kranitz K, Ahmed IIK, De Francesco T, Mikula E, Juhasz T. First-in-human safety study of femtosecond laser image-guided trabeculotomy for glaucoma treatment: 24-month outcomes. Ophthalmol Sci. 2023;3(4):100313.
40 Berlin MS, Shakibkhou J, Tilakaratna N, Giers U, Groth SL. Eight-year follow-up of excimer laser trabeculostomy alone and combined with phacoemulsification in patients with open-angle glaucoma. J Cataract Refract Surg. 2022;48(7):838-843. doi:10.1097/j.jcrs.0000000000000856
5. Grippo TM, de Crom RMPC, Giovingo M, et al. Evidence-based consensus guidelines series for micropulse transscleral laser therapy: dosimetry and patient selection. Clin Ophthalmol. 2022;16:1837-1846. doi:10.2147/OPTH.S365647
6. Grippo TM, Töteberg-Harms M, Giovingo M, et al. Evidence-based consensus guidelines series for micropulse transscleral laser therapy - surgical technique, post-operative care, expected outcomes and retreatment/enhancements. Clin Ophthalmol. 2023;17:71-83. doi:10.2147/OPTH.S389198









